

Treatment for deep vein thrombosis (DVT) aims to prevent the clot from growing larger, reduce the risk of complications such as pulmonary embolism (PE), and alleviate symptoms. Here’s an overview of the treatment options and strategies commonly used for managing DVT:
. Anticoagulant Medications
Complications and Considerations
Conclusion
Effective management of deep vein thrombosis requires a tailored approach based on the severity of the clot, presence of symptoms, and individual health factors. Early diagnosis, prompt initiation of anticoagulant therapy, and appropriate follow-up are crucial for reducing complications and improving outcomes in patients with DVT. Lifestyle modifications and adherence to treatment recommendations play key roles in preventing recurrence and promoting overall vascular health.
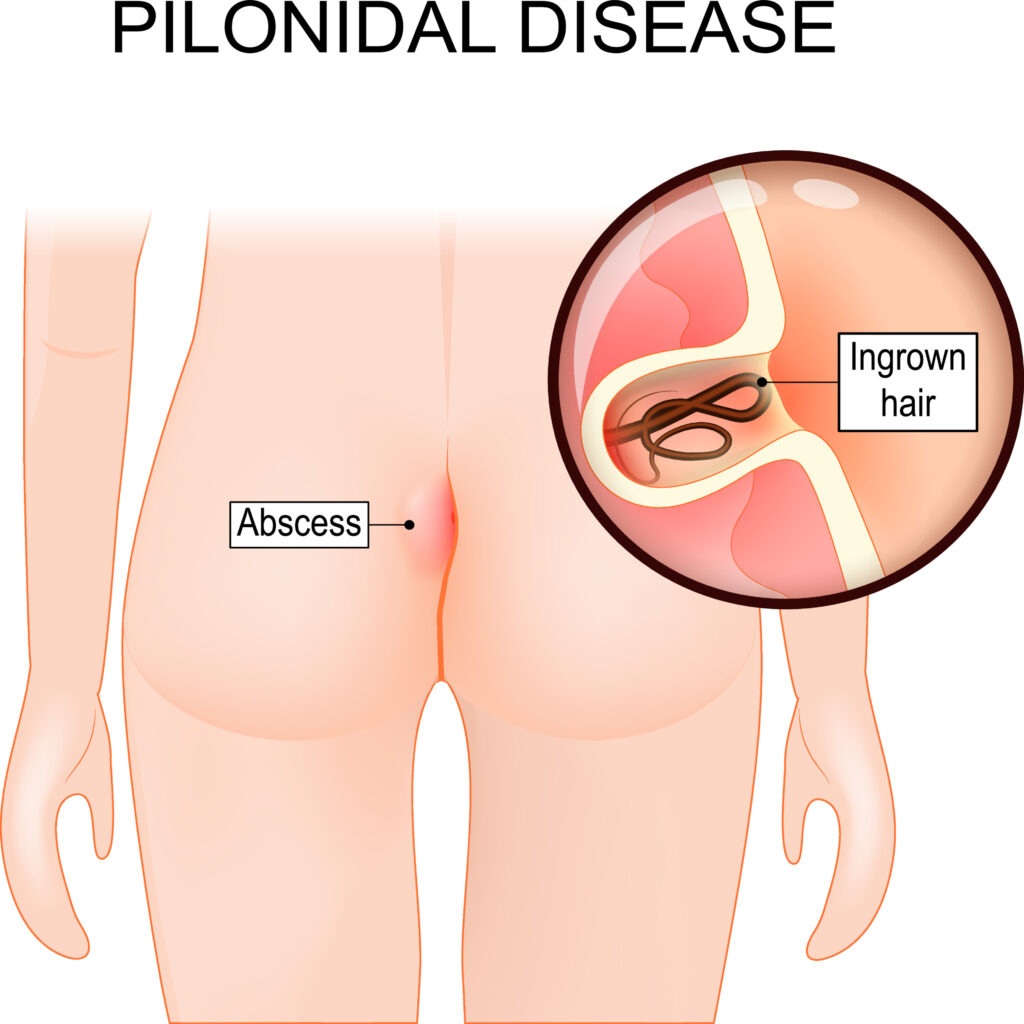
Pilonidal Sinus Surgery
Pilonidal sinus surgery is performed to treat a pilonidal sinus, a small cyst or abscess that occurs in the cleft at the top of the buttocks. This condition often involves infection and can cause significant discomfort. Here’s an overview of the surgical treatment for a pilonidal sinus, including indications, types of surgery, the procedure, and postoperative care:
Indications
Surgical intervention is indicated for:
Types of Pilonidal Sinus Surgery
There are several surgical options for treating a pilonidal sinus, ranging from minimally invasive procedures to more extensive surgeries:
Procedure Steps
Risks and Complications
Conclusion
Surgical treatment for pilonidal sinus aims to remove the infected tissue and prevent recurrence. The choice of surgical technique depends on the individual case, with considerations for the patient’s health, the extent of the disease, and the surgeon’s expertise. Proper postoperative care, including wound management and follow-up, is crucial for a successful outcome and to minimize the risk of complications.